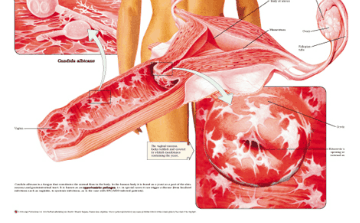
Vaginal infections, or vaginitis, are very common — so much so that most women will experience some form of vaginal infection or inflammation during their lifetime. Characterized by extremely uncomfortable itching, burning and pain, and discharge, vaginal yeast infections are most often caused by unhealthy forms of fungus that grow in the warm, damp environment of the female genitalia. Men may also experience this condition, but it is most common in women. The most prominent form of yeast infection fungus is Candida albicans.
The most common type of vaginitis, a yeast infection is caused by one of the many species of fungus known as Candida. Candida live naturally in your body in small numbers, including in the vagina, and usually don’t cause any harm. However, Candida thrive in a warm, moist, airless environment and, under those conditions, can grow in number, causing a vaginal infection.
Along with yeast, “friendly” bacteria called lactobacilli live in the vagina. When the number of lactobacilli gets too low, it can trigger a condition called bacterial vaginosis (BV). Why bacteria levels change is not known, but the normal lactobacilli can be replaced by other infection-causing bacteria.
Commonly called “trich,” – trichomonas vaginitis is caused by a single-celled parasite, trichomonas vaginalis, and is passed from partner to partner during intercourse. The symptoms of trichomonas vaginitis are similar to other vaginal infections: burning, irritation, redness, and swelling of the vulva, with a yellow-gray or greenish vaginal discharge, possibly with a fishy odor. Some women also experience pain during urination.
There are a number of treatment options for a vaginal yeast infection, including non-prescription vaginal medicine, prescription oral or vaginal medicine, or non-prescription vaginal boric acid capsules. The risk of self-treatment is that your symptoms may be caused by another vaginal infection, such as a sexually transmitted infection (STI), that requires different treatment. If you may have been exposed to an STI, it is best to discuss your symptoms with your doctor before using a non-prescription medicine. Your doctor may recommend testing for STI if you have risk factors for these infections.
One should keep in mind the following things
 Use pads instead of tampons while you are using nonprescription vaginal medicines. Tampons can absorb the medicine.
Use pads instead of tampons while you are using nonprescription vaginal medicines. Tampons can absorb the medicine.
Avoid using soap when cleaning the vaginal area-rinse with water only.
If sexual intercourse is painful, avoid it. Otherwise, use a water-soluble lubricating jelly (such as K-Y Jelly) to reduce irritation.
If the genital area is swollen or painful, sitting in warm water may help. Or instead, you may try putting a cool, damp cloth on the area. Do not rub to try to relieve itching.
There’s better evidence that probiotics may be the secret behind a diet to prevent yeast infections. Normally, certain bacteria live in the digestive tract, on the skin, and elsewhere on the body, where they help with digestion and other bodily functions.
A good way to help restore the body’s normal bacterial balance is through the consumption of probiotics. The best sources of probiotics are: Organic yogurt with live bacterial cultures
Supplements that contain bacteria — look for the words lactobacillus and/or acidophilus on the product. The amount of probiotics in any of these products can vary widely, so it is recommended that one reads the labels carefully before buying.
Do you want to find an effective Candida treatment? Check out our top rated Candida products